Oxygen Use with ALS
At some point in ALS progression the question of using oxygen to ease breathing difficulty will come up. Getting enough oxygen is not a the problem in ALS. There is nothing wrong with the lungs. The problem is muscle weakness that prevents inhaling deeply enough to get enough air in. If a machine such as a Bi-level Ventilator or an invasive ventilator is used to push enough air in, the lungs can absorb oxygen from room air without difficulty. Therefore the treatment for breathing problems in ALS is mechanical support, not oxygen. For people with ALS who also have lung problems that directly affect the ability of the lungs to absorb oxygven (such as pneumonia, COPD, emphysema or asthma) in addition to ALS, oxygen may be necessary.
Often the response to the use of oxygen is that it is dangerous for ALS patients. That is both true and false!
Respiratory drive runs on CO2 levels. Oxygen levels contribute very little to the process of stimulating breathing. CO2 is produced by working cells and sent through the blood to the lungs to be removed during the process of breathing. The CO2 is exchanged for oxygen and the CO2 is exhaled. When that exchange is impaired, CO2 levels rise and the respiratory regulatory center in the brainstem coordinates an increase in breathing rate and depth to blow it off. An ALS patient with weak respiratory muscles can't breathe deeper so the CO2 levels are harder to bring down.
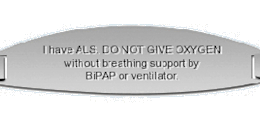
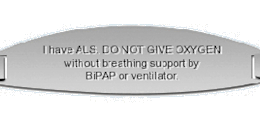
The risk of giving oxygen to an ALS patient who has high CO2 levels is not recognized by some
doctors and respiratory therapists. If you develop breathing problems and call for an ambulance or
go to the Emergency Room, protect yourself by wearing a Medic Alert bracelet. They are available
online from several companies. This site offers a range of styles.
medical-id-bracelets
The suggested wording is shown.

 Over time body chemistry allows the respiratory system compensate and to work with these
levels as the "new normal". When the compensatory measures are maxed out by increased weakness
of the respiratory muscles or lung congestion or pneumonia, that small amount of respiratory
drive from oxygen becomes helpful. But as oxygen is given and the O2 Saturation increases
to about 90%, that part of the respiratory drive stops because the O2 level is near normal. Loss
of that small part of respiratory drive is enough to tip the drive from "barely enough" to "not
enough". The rate of failure begins to increase and the patient may stop breathing entirely. The
risk of adding O2 is therefore very real—but only if the patient is retaining CO2 enough to
rely on compensatory body chemistry.
Over time body chemistry allows the respiratory system compensate and to work with these
levels as the "new normal". When the compensatory measures are maxed out by increased weakness
of the respiratory muscles or lung congestion or pneumonia, that small amount of respiratory
drive from oxygen becomes helpful. But as oxygen is given and the O2 Saturation increases
to about 90%, that part of the respiratory drive stops because the O2 level is near normal. Loss
of that small part of respiratory drive is enough to tip the drive from "barely enough" to "not
enough". The rate of failure begins to increase and the patient may stop breathing entirely. The
risk of adding O2 is therefore very real—but only if the patient is retaining CO2 enough to
rely on compensatory body chemistry.
The suggested wording is shown.